THANK YOU FOR VISITING SWEATSCIENCE.COM!
My new Sweat Science columns are being published at www.outsideonline.com/sweatscience. Also check out my new book, THE EXPLORER'S GENE: Why We Seek Big Challenges, New Flavors, and the Blank Spots on the Map, published in March 2025.
- Alex Hutchinson (@sweatscience)
***
Alcohol puts you to sleep — but how good is that sleep? A new study by Japanese researchers (abstract here; press release here) offers some interesting insights. Basically, it helps you get to sleep more quickly, and you sleep deeply for the first few hours, but once the “sedative and hypnotic effect of ethanol” wears off, it messes up the rest of the night and interferes with recovery.
The researchers studied 10 male university students. Each of them did three tests: one with a placebo, one with 0.5 grams of ethanol per kilogram of bodyweight, and one with 1.0 grams. The high dose corresponds to about four standard bottles of 5% beer for someone weighing 70 kg. They drank the beverages 100 minutes before bed, and then their sleep patterns were recorded.
Some background: your body is regulated by a balance between the “parasympathetic” nervous system (responsible for “rest-and-digest” functions) and the “sympathetic” nervous system (responsible for “fight-or-flight” functions). When you’re asleep, the parasympathetic system is supposed to take over and become dominant, helping your body to recover from the rigours of the day. What the Japanese study found for the first time (primarily by measuring heart rate and heart-rate variability) is that alcohol suppresses parasympathetic activity during sleep in a dose-dependent way (i.e. the higher dose of alcohol suppressed parasympathetic activity more strongly than the lower dose). The upshot:
These results suggest that ethanol disturbs the restorative effects of sleep, preventing the heart rate from decreasing and the parasympathetic nerves from becoming dominant. During the last half of the sleep period, when the sedative and hypnotic effect of ethanol wears off, the number of awakenings during sleep and Stage 1 increased under the [high dose] conditions.
Or, from the press release:
“It is generally believed that having a nightcap may aid sleep, especially sleep initiation,” said Nishino. “This may be true for some people who have small amounts of alcohol intake. However, it should be noted that large amounts of alcohol intake interfere with sleep quality and the restorative role of sleep and these negative consequences may be much larger during chronic alcohol intake.”
Bottom line: much like the effects of alcohol on muscle recovery, a few drinks isn’t likely to hurt you (and plenty of evidence suggests that a drink or two a night will improve your health). But more than that can affect your health in subtle ways that you probably don’t even notice.


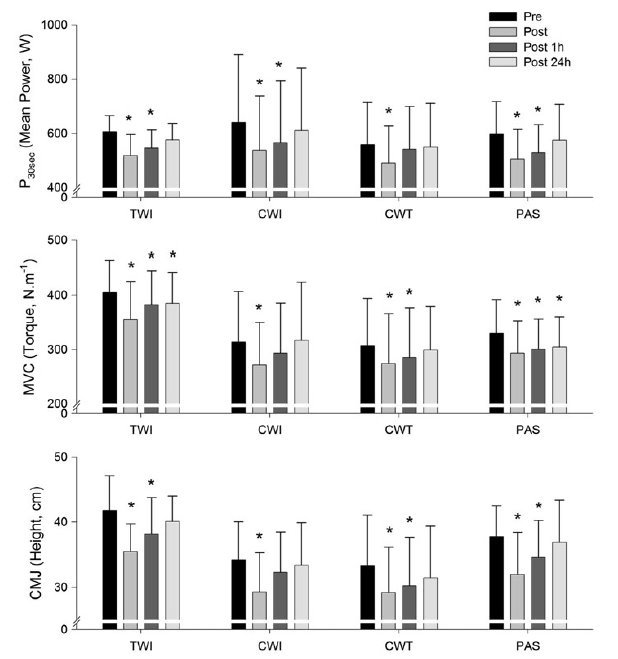
 This is the data for creatine kinase, which is a commonly measured marker related to muscle damage. Its exact significance is often debated, but the authors of this study suggest it’s a sign of “reduced passive leakage from disrupted skeletal muscle, which may result in the increase in force production during ensuing bouts of exercise.” The key: the ice bath outperforms all the other interventions, including the contrast bath.
This is the data for creatine kinase, which is a commonly measured marker related to muscle damage. Its exact significance is often debated, but the authors of this study suggest it’s a sign of “reduced passive leakage from disrupted skeletal muscle, which may result in the increase in force production during ensuing bouts of exercise.” The key: the ice bath outperforms all the other interventions, including the contrast bath.