THANK YOU FOR VISITING SWEATSCIENCE.COM!
As of September 2017, new Sweat Science columns are being published at www.outsideonline.com/sweatscience. Check out my bestselling new book on the science of endurance, ENDURE: Mind, Body, and the Curiously Elastic Limits of Human Performance, published in February 2018 with a foreword by Malcolm Gladwell.
- Alex Hutchinson (@sweatscience)
***
I was reading a profile of British historian Lucy Worsley in the New Yorker last night, in which the writer (Lauren Collins) takes part in the authentic re-enactment of the meal eaten by King George on February 6, 1789:
THEIR MAJESTIES DINNER
Soupe barley
4 chickens roasted
3 pullets minced and broiled
7 3/4 mutton collop pyes
6 perch boiled
2 breasts of lamb a la pluck
2 salmic of ducks
13 loin veal smort
(And a partridge in a pear tree, presumably.) The article is both fascinating and funny, but the culinary payoff after an enormous amount of work ends up being a bit anticlimactic:
If every age has its sounds and smells, it also has its flavors. The taste of 1789 can be a dog whistle to modern palates… “You’ve had your tongue burnt off by a Mexican chili, and you’ve been eating sugar cookies since you’ve been able to stand [says Marc Meltonville, co-head of the Historic Kitchens team;] if something’s subtle, sweetened with rose petals, how are you going to be able to taste it?”
This made me think of the long-running and bitter debate about the “right” amount of salt consumption, and how tastes are formed. Just this morning, the New York Times reported on a neat new study suggesting that the amount of salt you’re fed as an infant determines your taste for it in later life. But taste for salt is also somewhat plastic. When my wife and I started eating together, her taste for salt was dramatically higher than mine. Now, a few years later, our tastes have sort of met in the middle. She no longer adds as much salt to food as she used to; but when I visit my parents, I find that I now need to add salt to dishes that I loved for many years with no added salt.
And I still struggle to reconcile all this with the widespread message that we’re eating wayyy more salt now than we used to (and thus salt is responsible for the current epidemic of hypertension). As I wrote last year about a study by Harvard’s Walter Willett:
He and a colleague reviewed studies between 1957 and 2003 that measured sodium excretion in urine — a very accurate way of determining salt intake that gets around the difficulties in figuring out exactly how much salt is in your food. They found two main things: (a) sodium intake averaged about 3,700 mg per person per day, which is way higher than the upper recommended limit of 2,300; and (b) it essentially hasn’t changed in the half-century studied.
Interestingly, these results agree almost exactly with similar reviews of studies from 33 different countries: salt intake is high, and it hasn’t changed in recent memory.
And Henry VIII, according to Worsley in the New Yorker piece, ate 20 grams of salt each day!


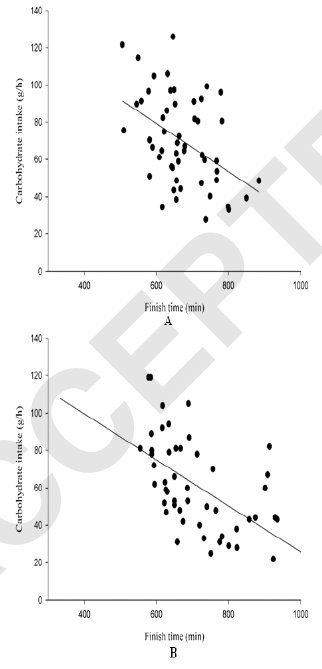 What do you see? A bunch of dots scattered randomly? Look a bit more closely. The data shows total carb intake (in grams per hour) by racers in Ironman Hawaii (top) and Ironman Germany (bottom), plotted against finishing time. It comes from
What do you see? A bunch of dots scattered randomly? Look a bit more closely. The data shows total carb intake (in grams per hour) by racers in Ironman Hawaii (top) and Ironman Germany (bottom), plotted against finishing time. It comes from